Understanding the Impact of Aging on the Cardiovascular System
As you age, the body undergoes various changes, including those that affect the cardiovascular system. Understanding these changes and their implications for your overall health and well-being is important. This article will explore the basics of the cardiovascular system, the aging process, its direct impact on the cardiovascular system, and common cardiovascular diseases in the elderly. It will also discuss the importance of preventing and managing cardiovascular health in aging.
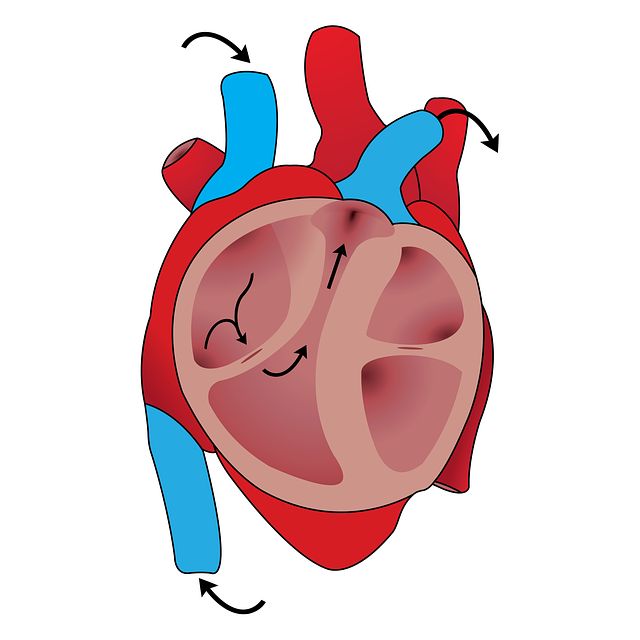
ALT TXT IMG: The heart
The Basics of the Cardiovascular System
The cardiovascular system, or circulatory system, is responsible for transporting blood, oxygen, and nutrients throughout our bodies. It consists of the heart, blood vessels, and blood. The heart acts as a pump, circulating blood to all parts of the body through a network of blood vessels, including arteries, veins, and capillaries.
The cardiovascular system is an intricate network that is crucial in maintaining your overall health. Without it, your body would not receive the necessary oxygen and nutrients needed for survival. Here is more on the fascinating world of the cardiovascular system.
The Heart’s Role in the Cardiovascular System
The heart is a vital organ that continuously beats, pumping blood to all areas of the body. It consists of four chambers – two atria and two ventricles – that work together to ensure efficient blood flow. The atria receive blood from the body and lungs, while the ventricles pump the blood out to the rest of the body.
But did you know that the heart is not just a mechanical pump? It is a complex organ that is intricately connected to emotions. Your heart rate can increase or decrease when you experience strong emotions such as love or fear. This connection between emotions and the heart is a testament to the intricate nature of the cardiovascular system.
As you age, the heart may undergo certain changes that can impact its function. Conditions such as high blood pressure, heart disease, and arrhythmias can affect the heart’s ability to pump blood effectively. Taking care of your cardiovascular health through regular exercise, a balanced diet, and regular check-ups with a healthcare professional is important.
Blood Vessels and Circulation
Blood vessels are the network of tubes that carry blood throughout the body. Arteries carry oxygen-rich blood away from the heart, while veins carry oxygen-poor blood back to the heart. Capillaries are tiny vessels that connect the arteries and veins at the cellular level, allowing for the exchange of oxygen, nutrients, and waste products.
Imagine the intricate network of blood vessels running through your body, reaching every nook and cranny. It is like a vast highway system, ensuring that every cell receives the necessary oxygen and nutrients it needs to function properly. Without this intricate network, your body would not be able to survive.
As you age, the efficiency of blood circulation can be affected. The walls of your blood vessels may become less elastic, making it harder for blood to flow smoothly. This can lead to conditions such as high blood pressure or even blockages in the arteries, which can have serious consequences for your health.
It is essential to maintain a healthy lifestyle to support optimal blood circulation. Regular exercise, a balanced diet rich in fruits and vegetables, and avoiding smoking can all contribute to keeping the cardiovascular system in top shape.
In conclusion, the cardiovascular system is a remarkable network that ensures the proper functioning of our bodies. Every component is vital in maintaining your overall health, from the beating heart to the intricate blood vessels. By understanding the basics of the cardiovascular system, you can take steps to care for it and enjoy a healthier life.
The Aging Process and Its General Impact on Health
As you age, the body undergoes various biological changes that can impact your overall health. Both genetic and environmental factors may influence these changes. It is important to understand the general impact of the aging process to ensure optimal health and well-being.
One of the most noticeable biological changes that occur with age is a decrease in muscle mass. This can lead to a loss of strength and mobility, making everyday tasks more challenging. Additionally, the stiffness of joints tends to increase as you age, making movements less fluid and causing discomfort.
Furthermore, hormonal changes play a significant role in the aging process. As you age, the production of certain hormones, such as estrogen and testosterone, decreases. This can have various effects on the body, including changes in mood, energy levels, and sexual function.
In addition to these internal changes, the decline in organ function is another common aspect of aging. Organs such as the heart, lungs, and kidneys may not work as efficiently as they did in your younger years. This can lead to a higher risk of developing chronic conditions and diseases.
Biological Changes with Age
With age, various changes occur in your body. These changes can include a decrease in muscle mass, increased stiffness of joints, hormonal changes, and a decline in organ function. The cardiovascular system is not immune to the effects of aging.
When it comes to the cardiovascular system, aging can have significant implications. The walls of blood vessels may become thicker and less elastic, leading to a decrease in blood flow and an increased risk of high blood pressure. Additionally, the heart muscle may weaken over time, making it harder for the heart to pump blood efficiently.
It is important to note that the aging process affects individuals differently. While some people may experience these changes more prominently, others may age more gracefully with minimal impact on their health. Genetics, lifestyle choices, and overall health play a role in how the aging process unfolds for each individual.
Lifestyle Factors Influencing Aging
“Movement is a medicine for creating change in a person’s physical, mental, and emotional state.”
-Carol Welch
Lifestyle factors, such as diet, physical activity, smoking, and stress, can also influence the aging process. Poor lifestyle choices can accelerate the aging process and increase the risk of developing cardiovascular diseases. Therefore, adopting healthy lifestyle habits is crucial for maintaining cardiovascular health as you age.
When it comes to diet, consuming a balanced and nutritious meal plan can provide the body with essential nutrients needed for optimal functioning. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help support overall health and slow down the aging process.
Regular physical activity is another crucial aspect of healthy aging. Engaging in moderate-intensity exercises, such as walking, swimming, or cycling, can help maintain muscle strength, flexibility, and cardiovascular health. Exercise also promotes the release of endorphins, which can improve mood and overall well-being.
Smoking, on the other hand, is a lifestyle choice that can significantly accelerate the aging process. Smoking damages the blood vessels, reduces lung function, and increases the risk of developing various diseases, including heart disease and cancer. Quitting smoking is one of the most impactful steps one can take to slow down the aging process and improve overall health.
Lastly, managing stress levels is essential for healthy aging. Chronic stress can have detrimental effects on both physical and mental health. Finding healthy coping mechanisms, such as practicing mindfulness, engaging in hobbies, or seeking support from loved ones, can help reduce stress and promote overall well-being.
In conclusion, the aging process brings about various biological changes that can impact your health. Understanding these changes and adopting healthy lifestyle habits can help mitigate the negative effects of aging and promote optimal well-being as you grow older.
ALT TXT IMG: Heart care
Aging and Its Direct Impact on the Cardiovascular System
Aging directly affects the cardiovascular system, leading to significant changes that can impact its function. It is important to be aware of these age-related changes to effectively manage cardiovascular health in the elderly.
Age-Related Changes in the Heart
As you age, the heart undergoes various changes. The walls of the heart may become thicker, the heart rate may slow down, and the heart’s ability to respond to physical stress may decrease. These changes can affect the heart’s overall efficiency and increase the risk of developing cardiovascular diseases.
One of the age-related changes in the heart is the thickening of its walls. This occurs due to the accumulation of collagen, a fibrous protein, in the heart muscle. The thickening of the heart walls can lead to a decrease in the heart’s ability to pump blood effectively, resulting in reduced cardiac output.
Another change that occurs in the aging heart is a decrease in the heart rate. This is mainly due to changes in the electrical conduction system of the heart. As you age, the cells responsible for generating electrical signals in the heart may become less efficient, leading to a slower heart rate. This can affect the heart’s ability to respond to physical stress and may result in symptoms such as fatigue and shortness of breath during exercise.
In addition to the changes in heart structure and function, the aging heart may also experience a decline in its ability to respond to physical stress. This means that the heart may not be able to increase its pumping capacity as efficiently during increased demand, such as during exercise or emotional stress. This reduced ability to respond to stress can increase the risk of cardiovascular events in the elderly.
Aging and Blood Vessels
Blood vessels also undergo age-related changes. Arteries may become stiffer and less elastic, reducing their ability to expand and contract. This can lead to increased blood pressure and decreased blood flow to vital organs. Additionally, the formation of plaques in the arteries (atherosclerosis) becomes more common with age, increasing the risk of cardiovascular diseases such as heart attacks and strokes.
One of the age-related changes in blood vessels is the loss of elasticity. Elasticity is an important property of blood vessels that allows them to expand and contract in response to changes in blood flow. With age, the elastic fibers in the arterial walls may become stiffer and less flexible, leading to decreased elasticity. This can result in increased resistance to blood flow and higher blood pressure.
Another age-related change in blood vessels is the formation of plaques in the arteries. Plaques are fatty deposits that build up on the inner walls of the arteries, narrowing the blood vessels and reducing blood flow. This process, known as atherosclerosis, becomes more common with age and can significantly increase the risk of cardiovascular diseases such as heart attacks and strokes.
Furthermore, the aging process can also affect the endothelial cells lining the blood vessels. These cells play a crucial role in maintaining the health and function of blood vessels. With aging, the endothelial cells may become less efficient in producing nitric oxide, a molecule that helps regulate blood vessel tone and prevents the formation of blood clots. This can further contribute to the development of cardiovascular diseases.
In conclusion, aging has a direct impact on the cardiovascular system, leading to various changes in the heart and blood vessels. These age-related changes can affect the overall function of the cardiovascular system and increase the risk of developing cardiovascular diseases. Understanding and managing these changes is crucial for maintaining cardiovascular health in the elderly.
Common Cardiovascular Diseases in the Elderly
With aging, the risk of developing cardiovascular diseases increases. It is important to be aware of these diseases to detect and manage them early, thus reducing the risk of complications.
Heart Disease and Aging
Heart disease, including conditions such as coronary artery disease, heart failure, and arrhythmias, is common in the elderly. These conditions can significantly impact cardiovascular health and require appropriate management to prevent complications.
Hypertension in the Elderly
Hypertension, or high blood pressure, is prevalent in the elderly population. It is important to regularly monitor blood pressure and manage it effectively to reduce the risk of cardiovascular diseases.
Prevention and Management of Cardiovascular Health in Aging
Prevention and management are key to maintaining cardiovascular health as you age. By adopting healthy lifestyle choices and seeking regular medical check-ups, you can reduce the risk of cardiovascular diseases and improve overall well-being.
Importance of Regular Check-ups
Regular check-ups with healthcare professionals, such as primary care physicians and cardiologists, are crucial for monitoring cardiovascular health and detecting any early signs of disease. These check-ups may include blood pressure measurement, cholesterol level screening, and other relevant tests.
Healthy Lifestyle Choices for Cardiovascular Health
Adopting a healthy lifestyle plays a pivotal role in maintaining cardiovascular health. This includes eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, engaging in regular physical activity, avoiding or quitting smoking, managing stress levels, and maintaining a healthy weight.
Conclusion
Understanding the impact of aging on the cardiovascular system is essential for maintaining optimal health and well-being as we grow older. By being aware of the changes that occur with age and adopting healthy lifestyle choices, you can reduce the risk of cardiovascular diseases and enjoy a fulfilling life. Regular check-ups and proactive management of cardiovascular health are crucial in preventing complications and ensuring a healthy aging process. Are you aging fast or slow? Take this test to find out.
Lastly, if you’re interested in going deeper on health-related content, here are a few of our recent posts that you may want to read:
- Why Optimized, Precision Medicine is the Future
- Andrew Huberman is Wrong About NAD, NAD+ precursor & Longevity
- 9 Powerful Benefits of Optimizing Your NAD
- What Does Peak Performance Look Like?
P.S. Want to boost your intracellular NAD levels? Try a 2 week trial of our Jinfiniti Vitality Boost (do 2 scoops per day), use the discount code Blog15 if you’re a new customer for 15% off your 1st order)